Striking NHSmedical professionals are using deceptive data to support their exorbitant salary requests, according to a study.
Residents are planning to halt hospital operations starting Friday, staging a five-day strike in their bid for salary increases of up to £20,000.
Union leaders involved in the conflict argue that the medical staff, who were once called junior doctors, require a salary increase of more than 29% to compensate for 17 years of reduced wages.
In addition to the average 28.9 per cent given to resident doctors in the past three years, this includes a significant increase of 5.4 per cent this year – the highest in the public sector.
Leaders of the British Medical Association (BMA) claim this is insufficient.
Health Secretary Wes Streetingcondemned the BMA’s strike action, describing it as ‘shockingly irresponsible’ and stating he will not compromise on pay.
The authorities state that the typical full-time starting salary for a resident doctor has reached £54,300. This marks an increase from approximately £42,000 in 2022/23.
If the BMA’s requirements are fulfilled, their typical starting salary would go beyond £70,000 annually. This would result in the highest-ranking resident doctors receiving an additional £20,000 compared to their 2024/25 earnings.
Ministers are still working towards an agreement to prevent further strike disruptions, which might involve forgiving part of doctors’ student loan debt to satisfy them.
Resident physicians have engaged in industrial action 11 times since the first discussions started in 2022.
The BMA’s campaign materials state that wage decreases have been 21 per cent lower than inflation since 2008/09.
On their website, the union states: ‘In other words, trainee doctors are still dedicating a fifth of their working hours without pay.’
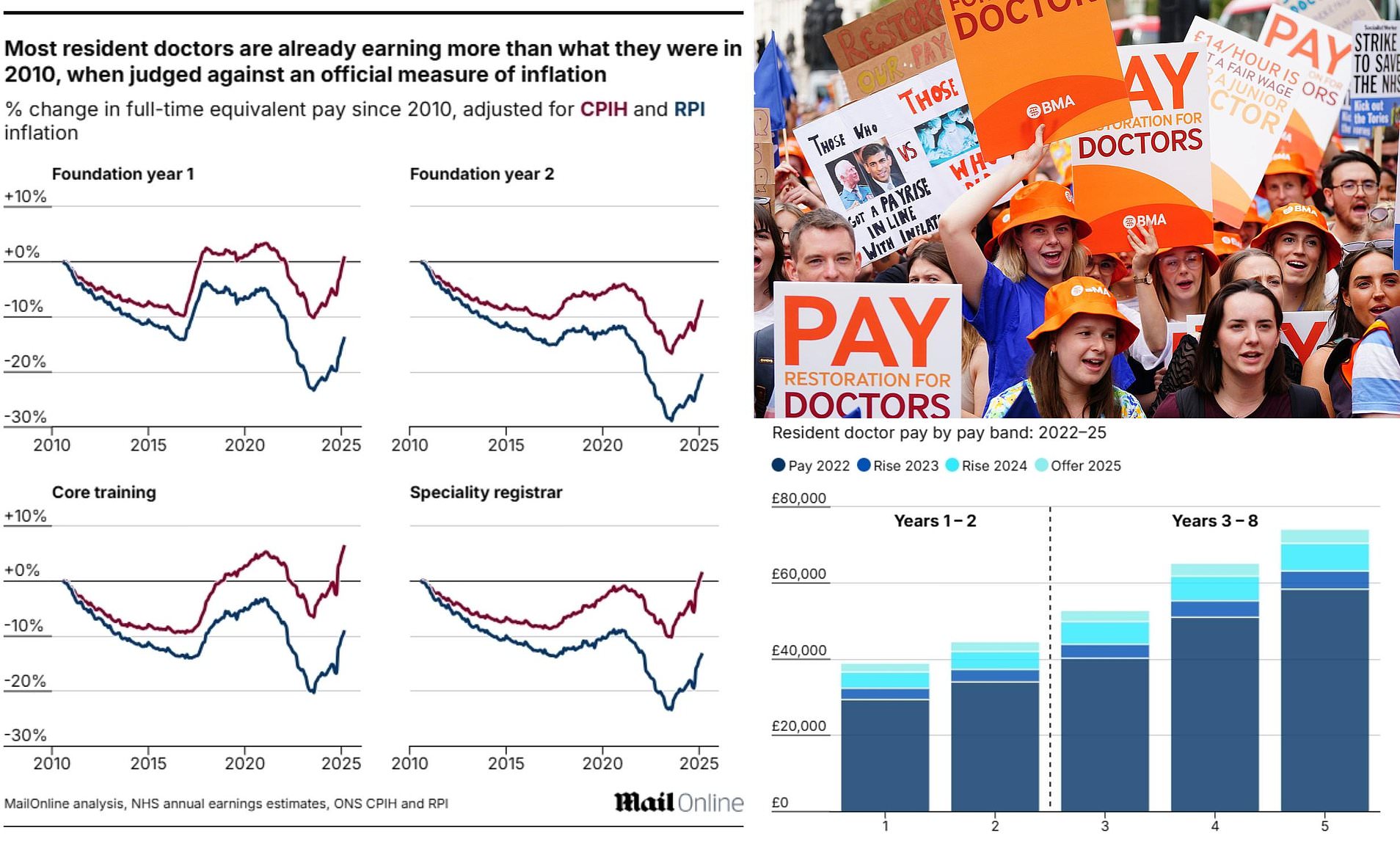
Nevertheless, this amount is determined based on the Retail Price Index (RPI) inflation indicator.
Monitoring the salaries of trainee doctors in relation to the Consumer Price Index (CPI), the Nuffield Trust discovered that they are only 4.7 per cent lower since 2008.
Tackling this decline would result in an average increase of approximately five per cent. This would translate to an average salary rise of less than £3,000.
In comparison to CPI figures from 2015/16, the Nuffield Trust found that trainee doctors have experienced a 7.9 per cent rise in their wages.
Official sources have criticized the BMA for using RPI in its calculations, as it exaggerates inflation.
As a result, the statistics authority reduced the status of RPI to an unofficial national measure in 2013. From that point onward, CPI and CPIH (CPI with housing costs included) have been the recognized benchmarks for measuring inflation.
MailOnline is aware that the Government plans to discontinue its usage by the end of the current decade.
Questioned about the salaries of other NHS employees, Mr Streeting told MPs that funds are ‘limited’.
He stated: “These kinds of decisions and compromises regarding resources are exactly why I requested BMA trainee doctors to recognize that, having received a 28.9 per cent salary increase from this government in the past year, they should be aware of the responsibility I hold, as well as their own responsibility towards some of their less well-paid colleagues.”
Resources are limited, and it’s crucial that I act in the best interests of every NHS employee, with special attention to those who put in a lot of effort but aren’t adequately recognized.
Nevertheless, the BMA has supported its application of RPI, contending that it is a more reliable measure for the general public.
A representative from the BMA stated: ‘RPI is a metric that, in alignment with the broader trade union sector, we feel most accurately captures the actual experiences of workers in the UK, and which the Government still employs when it is convenient.
Firstly, RPI determines student loan repayments. In a nation where newly qualified doctors frequently face student debts exceeding £100,000, this represents a significant portion of their expenses.
Car taxes and train ticket price limits are determined by RPI, forming a significant portion of the expenses for many doctors who end up with lengthy commutes due to their relocations across the country during rotations.
These actions also require securing accommodation, a expense that in turn influences the calculations of RPI and further enhances its significance for a working physician.
A MailOnline review indicates that the standard full-time equivalent (FTE) salaries for nearly all categories of resident doctors have increased over the last 15 years compared to the CPIH.
Only foundation year 2 (FY2) medical practitioners have experienced a reduction in earnings when considering the data in this manner.
In March 2025, the salaries of core training and specialty registrar doctors were 1.1%, 6.5%, and 1.7% higher, respectively, compared to August 2010, when considering CPIH inflation.
Our computations consider only base salary, meaning the roughly one-quarter of doctors’ earnings that comes from extra compensation—like overtime and additional payments for inconvenient working hours—is excluded.
In September, members of the BMA agreed to a government salary agreement that provides an average increase of 22.3 per cent over a two-year period.conclude a large amount of strike activitybothering the former Conservative government.
The 2025/26 salary agreement provided resident doctors with a 4 per cent increase along with an additional £750, all combined into a single payment.
This resulted in an average increase of 5.4 percent, adding up to 28.9 percent over the three-year period.
Nevertheless, this was not sufficient to prevent additional strike activity, as BMA members strongly supported new actions against the proposal. Almost 90 per cent of 30,000 doctors (with a 55 per cent participation rate) voted to go on strike.
A representative from the Department for Health and Social Care stated to MailOnline: ‘Trainee doctors have experienced the largest salary increases in the public sector for two consecutive years due to this government, with a rise of 28.9 per cent over three years.’
Support from the public for the strikes by resident doctors has declined, with most BMA resident doctors not casting their vote in favor of these actions.
Nuffield Trust researcher Lucina Rolewicz stated: ‘The real-term adjustments to resident doctors’ salaries over time can appear quite different, depending on the approach taken.’
It is crucial to examine various baseline years to gain a more comprehensive insight into changes in wages. For instance, when considering the developments since 2008, wage decline seems more severe compared to looking at changes since 2015 alone.
In contrast to the CPI inflation measurement, this could result in a 4.7 per cent decrease in wages since 2008 or a 7.9 per cent rise since 2015.

Examining adjustments to wages at the same time, with varying inflation indicators, leads to significantly different outcomes. For example, the salary of resident doctors has dropped by 4.7 per cent since 2008 according to CPI, yet has declined by 17.9 per cent during the same period when measured by RPI.
Considering the significance of the discussion for medical professionals, their peers, patients, and the public, it is essential that we examine every aspect in which remuneration has evolved.
It follows a report from yesterday that cautioned that impending strikes might result in 250,000 appointments being cancelled or delayed this month.
The Policy Exchange think-tank stated that the strikes could also result in the NHS losing £87 million for staff coverage.
Charities have voiced their ‘deep worry’ about the move and cautioned that it could lead to ‘considerable suffering, anguish, and deteriorating health among patients’.
Consultants may profit by imposing high fees of as much as £2,504 per shift to replace missing junior staff, draining hospitals of money that could have been directed towards purchasing new imaging equipment, fixing infrastructure or performing additional treatments.
Junior doctors have completed medical school but continue with clinical training for as long as eight years. They perform their duties under the guidance of more experienced physicians during their practical training.
Previous job actions by junior physicians resulted in fatalitiesat least five patients, an audit found last week.
NHS officials have cautioned that “additional lives might be endangered” throughout the upcoming five-day complete strike.