Understanding the Science Behind Obsessive Compulsive Disorder
Living with Obsessive Compulsive Disorder (OCD) is far more than just being overly neat or having a strong preference for order. It’s a complex mental health condition that affects millions of people worldwide, often causing significant distress and disruption in daily life. OCD isn’t about personality quirks or minor habits; it’s a real neurological condition rooted in the brain’s functioning.
At its core, OCD involves intrusive thoughts that feel overwhelming and persistent. These thoughts are not just random musings—they can be deeply unsettling, leading to compulsions that individuals feel compelled to perform in an attempt to ease their anxiety. The cycle of these thoughts and rituals can be exhausting, making it difficult for those affected to break free from the pattern.
The Brain’s Role in OCD
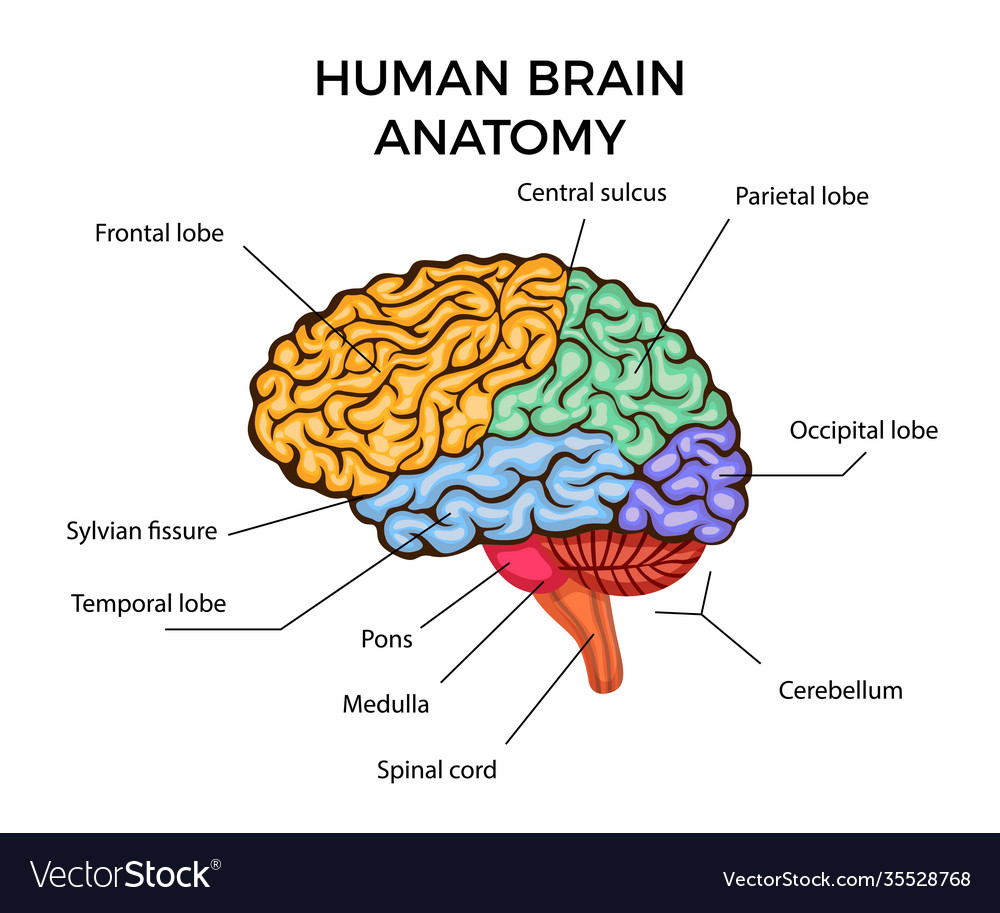
The brain plays a crucial role in the development and persistence of OCD. Normally, the brain has an alarm system that helps detect threats and protect us from danger. This system, involving areas like the amygdala, triggers a response when something dangerous is perceived. For example, if a child suddenly runs into the road, the brain quickly signals to stop and avoid harm.
In people with OCD, this alarm system becomes overactive. It doesn’t switch off properly, even when there is no actual threat. This leads to a heightened sensitivity to potential dangers, which can result in intrusive thoughts that feel very real. These thoughts might include fears like “What if I left the gas on?” or “What if I did something terrible without knowing?”
This misfiring of the brain’s threat detection system is similar to a smoke alarm that goes off every time you boil water or light a candle. The brain can’t distinguish between a real threat and an everyday situation, leading to constant worry and the need to perform compulsions to alleviate the anxiety.
The Neurological Mechanisms
The brain’s “error detector,” known as the orbitofrontal cortex, is responsible for identifying potential mistakes or dangers. In individuals with OCD, this area constantly sends out false alarms, even when there is no real threat. Additionally, the caudate nucleus, which acts as a filter, fails to turn off these alarms properly. As a result, the same worries and fears repeat themselves, creating a loop that is hard to escape.
This mechanism explains why intrusive thoughts feel so real and why individuals feel forced to engage in compulsions. The brain believes there is a danger, even though logically, there may not be one. The relief from performing the compulsion is only temporary, and the cycle continues, reinforcing the brain’s belief that the threat is real.
Causes and Triggers
OCD can have multiple causes, including genetic factors. Research suggests that it can run in families, indicating a possible hereditary component. Additionally, certain parts of the brain may function differently in individuals with OCD, contributing to the condition.
Life events such as stress, trauma, or significant changes can also trigger OCD symptoms, especially in those who are already prone to anxiety or perfectionism. Brain scans have shown differences in the way certain circuits communicate in people with OCD, resembling a glitchy light switch that won’t turn off.
Treatment and Hope
Despite the challenges, there is hope for individuals living with OCD. Therapy, particularly cognitive-behavioral therapy (CBT), can help people face their fears without giving in to compulsions. Medications can also play a role in reducing the intensity of intrusive thoughts and calming the anxiety that fuels the cycle.
It’s important to remember that OCD is not something people choose. It’s a neurological condition that requires understanding, support, and treatment. With the right approach, individuals can learn to manage their symptoms and regain control over their lives.
Rebuilding Trust and Healing
Healing from OCD takes time, patience, and self-compassion. The brain can rewire itself through therapy, helping individuals confront their fears without engaging in compulsions. Over time, the brain learns that nothing bad happens when these thoughts are faced, and the alarm begins to quiet down.
For those struggling with intrusive thoughts and compulsions, it’s essential to seek professional help. Support from loved ones and mental health professionals can make a significant difference in the journey toward recovery.
OCD is treatable, and many people find ways to live fulfilling lives despite the challenges. With the right tools and support, individuals can break free from the cycle and reclaim their sense of safety and control.