UK Government Considers Prioritizing Home-Trained Doctors to Prevent NHS Strikes
The UK government is exploring ways to give greater priority to doctors trained in the country for NHS jobs as it works to avoid a potential wave of strikes by resident doctors later this month. This move comes as part of broader efforts to address concerns over workforce shortages and working conditions within the healthcare system.
As part of its long-term 10-year plan for the NHS, the government has pledged to limit the number of overseas recruits to no more than one in ten. This initiative aims to reform a system that currently relies heavily on international doctors, with two-thirds of new hires coming from abroad. However, ministers are reportedly considering further measures to address the ongoing dispute with the British Medical Association (BMA), which represents resident doctors—formerly known as junior doctors.
In 2020, during the height of the pandemic, then-Health Secretary Matt Hancock expanded the competition for training posts to include global applicants, exacerbating the challenge of securing positions for local doctors. This has led to increased competition, slowing career progression for many professionals. The government may look to address this bottleneck as part of negotiations over the upcoming strikes.
In addition to tackling the issue of job availability, the Health Secretary, Wes Streeting, is reportedly open to discussing other aspects of working conditions, such as annual leave and specialty rotations. These discussions could play a key role in resolving the current impasse.
Despite the BMA’s public stance against certain proposals, insiders suggest that the idea of cutting doctors’ pension pots to boost pay is still under consideration. While the union has ruled out this option publicly, some believe there is potential for compromise on other issues.
One insider noted that “there is enough common ground” to reach an agreement on working conditions, even if the two sides remain divided on pay. They emphasized that “there are lots of areas where we agree,” indicating that progress might be possible in these discussions.
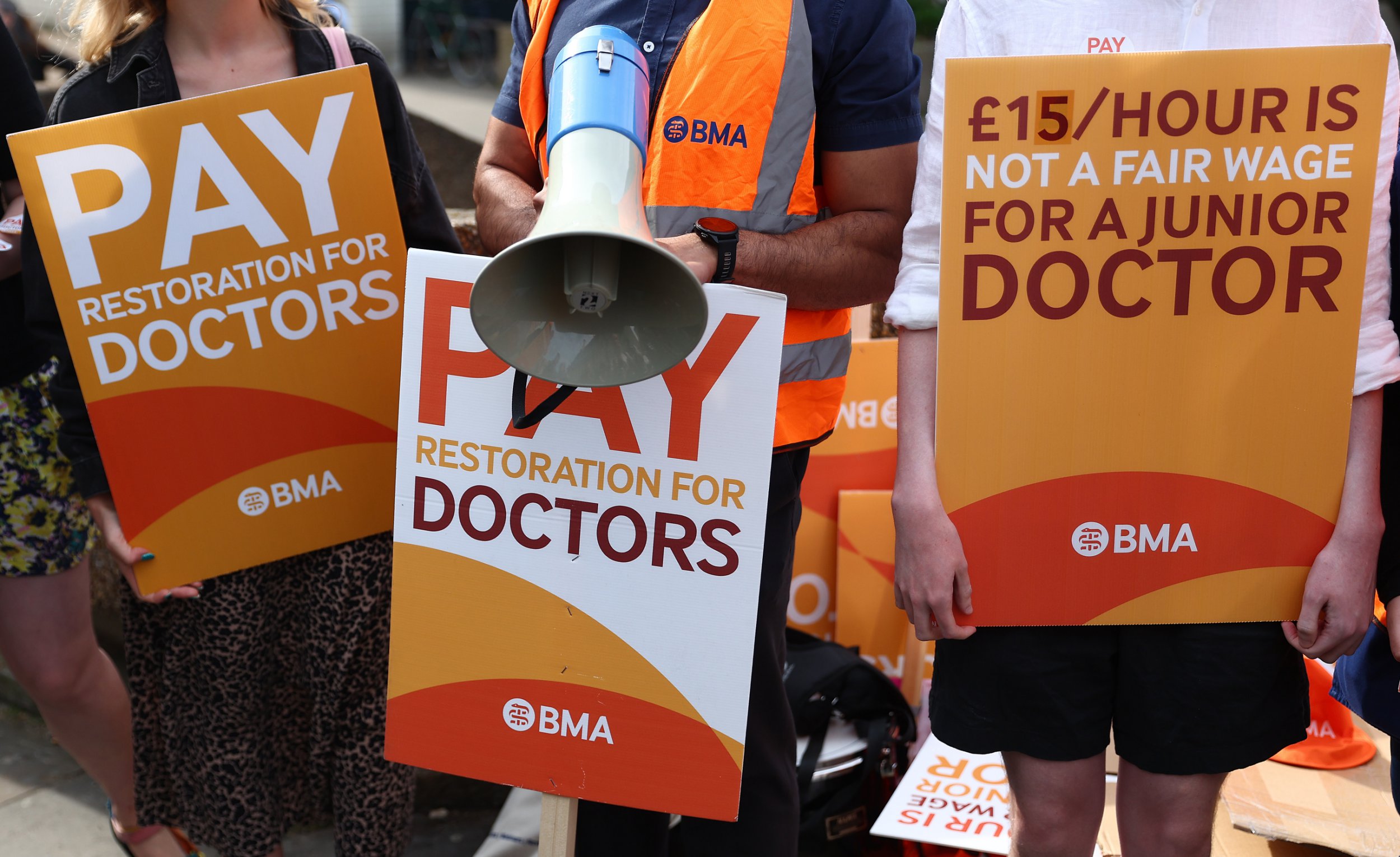
Resident doctors are set to walk out between 25 and 30 July over pay disputes. The BMA is urging the government to improve on its 5.4% pay offer for this financial year, arguing that real-term pay has dropped by 20% since 2008. However, the government has stated it cannot increase the offer, but is open to concessions on working conditions.
Streeting recently wrote to the BMA, stating: “While we cannot go further on pay this year, there is so much more we can do together to improve the lives of resident doctors and the wider NHS.” This conciliatory tone highlights the government’s willingness to explore alternative solutions.
Concerns Over Impact of Strikes on NHS Services
Insiders are increasingly worried about the potential impact of the strikes on NHS services. Reports suggest that NHS trusts are uncertain about how many trainee doctors may walk out, making it difficult to plan for adequate staffing. Some unions have instructed doctors not to inform their hospitals of their intention to strike, complicating efforts to manage coverage.
Historical data shows that previous strikes had significant effects on patient care. During 44 days of walkouts in 2023, cancer operations dropped by 31%, emergency heart surgeries fell by 13%, and delays were reported in neonatal and mental health care. With fewer warnings this time, the impact could be even greater.
The BMA has expressed willingness to engage in talks to prevent the strikes but insists that the government has yet to present a “credible” offer. While the union is open to discussing non-pay issues, it maintains that the core issue remains pay erosion and that insufficient progress has been made to restore salary value.
In a recent letter to Streeting, seen by The i Paper, the BMA stated: “We are committed to meeting with you to settle our dispute and avoid strike action.” However, it criticized the government for not addressing pay concerns or identifying non-pay issues for discussion. The union also pointed out that previous commitments, such as improvements to training rotations and exception reporting, have not been fulfilled.
The BMA highlighted that the review into rotational training has barely started and that the small increases in training places announced in the NHS workforce plan do not adequately address the immediate crisis. This suggests that more needs to be done to support the next generation of doctors and ensure the sustainability of the NHS.